Every Tuesday and Thursday morning, at 9:30 am, I meet up with a group of friends. We’re not meeting for breakfast or coffee or anything that would require talking to each other. Instead, we meet at the Boulder Centre for Orthopedics. Actually, these people I’m speaking of have no idea they’ve become a part of my twice a week circle or that I’d refer to them as “friends.” It’s best that way. It started the first time I did PT on site – week 3 post op. I arrived 15 minutes early because I always arrive places 15 minutes early. I’ve still not gotten used to the fact that Boulder is a much smaller town than I’m used to and it never takes me as long as I anticipate to get from place to place. As I sat in the lobby area that held a dozen or so chairs and looked out onto the open area with exercise bikes, weights, portable steps and a reformer-like machine, I did what I always do. I people watched, which is what I call it as it doesn’t sound as rude as blatant staring. This time and place felt different from my usual “spying” because I could see that I had something in common with many people in the room, namely the ones in shorts who were exercising a new knee. Watching them, OK, spying on them, has given me the opportunity of seeing either what’s next for me in my knee journey, or taking pride in how far I’ve come when I see the new patients, still in their hospital issued, white, and terribly unattractive, support hose. If I’m close enough to see either the steri-strips or the vertical scar that runs the distance of the knee cap, I take note because we’re members of the same club.
On my first visit, I still had the stere-strips lined up over my incision and was using a cane. A month later, in the same lobby, I’m drawn to the patients that come in (in shorts) that are using a walker or a cane, also with the steri-strips evenly spaced down the long incision. I know the pain they are in and I know the fear they will experience when the compass-like measuring device comes out because I’ve been there and it wasn’t that long ago. They have become my measuring stick for how far I’ve come. It’s a necessary part of recovery because sometimes, especially on a bad day, it’s hard to remember those days of maneuvering up and down the two steps that connect my kitchen to my living room. It’s also important for me to see the patients whose knee scar is a faint line and who are doing high reps of deep squats. They are ahead of me. They are my goal.
I’m gathering information. I’m in detective mode.
A few days ago, while working on some balancing exercises with my therapist, Esther, she told me (nicely) that I needed to focus on what I was doing. I told her I agreed whole heartedly but was a bit distracted at the moment. A police officer with a shackled prisoner in an orange jump suit, were making their way to the other side of the room, passing just feet away from where we were working. I realized I was staring, full on, wide eyed and with my mouth dropped open. Esther didn’t seem to be as distracted as I was, which indicated to me she had seen this before. She stopped counting reps and explained.
“We get prisoners on occasion who need physical therapy. Usually on their hands. If a hand injury isn’t treated soon, mobility is lost.”
“How do they injure their hands,” I asked, wanting to dig into every detail of the strange and somewhat uncomfortable situation that was unfolding in front of me.“I don’t know… well, I have ideas about it… maybe from punching people?? But I can’t say for sure,” Esther answered.
The police officer and his prisoner moved to the back of the room where the prisoner sat down at a table and a therapist took her place on the opposite side. I couldn’t see what was going on, but assumed it was the hand therapy Esther had spoken of. Unfortunately, once I had completed the exercised, Esther, had me move to a different area to work and I lost my view of what was far more interesting than people limping in with canes or walkers on what I guessed were 3 week old, knees.
Yesterday, I saw a man walk into the physical therapy room with slow, measured steps. I was on the Exercycle, getting in my 30 minutes of warm up before my session when I saw him. He was wearing the hospital-issued white ted hose and was using a walker. I put him at 2 weeks out — long enough that he was driving (he was by himself) but not long enough that he could take the ted hose off. He looked like he was in pain and I knew exactly what that pain felt like. I wanted to shout out words of comfort to him, but also didn’t want to be creepy. Thankfully, someone beat me to it and casually told him as they walked past that it would get better. That person, also in shorts, with the long scar that ran vertically down his knee cap, had just finished a round of squats with his therapist. I’d put him at 2 months out. Ahead of me. I’m getting good at this.
I don’t know any of their names, nor do they know mine, but I am connected to this group because of the scars we share. I also know where they are in their journey. We all know, but it’s possible that the others aren’t as invested as I am with their spying followed by writing about it. I’ve been coming to this place for PT for a month, but it seems like a very long time ago that I was the new one in the room when I walked in for my first sesion. It was an assessment session, with no exercising, along with measuring my flexion and removing the stere-strips. That appointment opened my floodgates of emotional tears and an intimacy that my all business, not much fun therapist probably hadn’t expected. It was my last crying episode and now I spend my time trying to get Ingrid to engage with me rather than have her uncomfortably handing me a tissue. (Esther is her assistant and is much more talkative, but my sessions always begin with Ingrid.). On one of my first visits, I asked her when she thought we might have our first snow. Weather is always a good conversation starter (I’m from the midwest after all) and although I don’t care for small talk, I dove right in with my snow question. Her answer was brief and immediate.
“Depends on where you live. In the mountains, it will be sooner.”
I let it go and tried to redirect my attempts at conversation to something I thought might interest her more. I asked her if it’s hard if her patients don’t do the exercises or after a few weeks decide they don’t need to come any more. Bingo. I hit my target. For the first time, Ingrid was animated and began to share stories that confirmed my theory of the frustrations physical therapists face with some of their patients. That is what I now reach for when I’m tired of the silence as she massages my leg followed by the flexion measurement, which no longer has me bracing but instead, puts me in competitive mode as I want to beat my last measurement. For those who have gotten a knee replacement and are familiar with the measurement, I’m at 135, or about the same as my other knee. I’m thrilled. Today, I added another talking point – my Halloween costume. I described how I added my own “artificial knee” to a skeleton unitard, complete with a little stuffing to show some swelling. She loved it and insisted I get a picture of me in it and made me promise I would show it to Dr. Bowman at my next appointment, which happens to be in a few days. I figured he should get the credit, so added the tag. It could be a business booster for him.

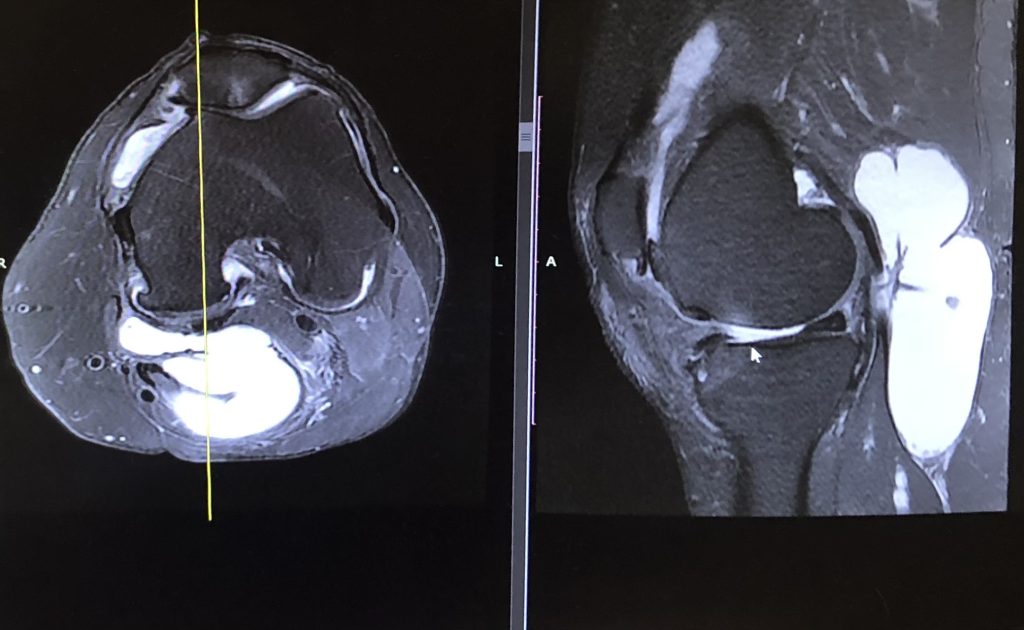
Exaggerated size and puffed up to show swelling, but my new knee really does look like a bikini (I used my X-Ray for reference…). Card says: “Knee by: Dr. Bowman”
As I was leaving my last appointment, a very fit man came in wearing shorts, with the telltale line running down his left knee, visible, but faint. As he and his therapist were walking back to one of the rooms, I heard the therapist say,
“We always have to tell our Boulderites that a a rest day is not a bad thing. It’s important and necessary.”
I couldn’t hear his response, but assumed the therapist’s words were directed at him. I did a quick assessment of my own rehab and recovery situation, wondering if I would fall into the “typical Boulderite” category of one who is pushing their way too hard and too fast towards recovery. For one, I drove to my physical therapy appointment, and didn’t ride my bike or roller blade or skateboard or any number of ways people in my very fit town navigate their way from one place to another. No, I’m good. I do my daily walk(s), my exercises and hop on an exercise bike at the gym for 30 minutes several times a week. I also feel no guilt if I want to chuck it all and sit on my couch and watch old movies or reruns of Friends. Those days don’t happen often, but when they do, I get the ice and the pillows for elevation and embrace them, remembering the therapist’s words about rest days. I’m an obedient patient.